…Writing a Different Story
NavigationA Ray of Hope
A Ray of Hope: DHA Therapy and Nutrition
Since DHA is so important for the developing brain and retina, for ethical reasons, we think that all the patients should be treated, disregarding phenotype and age. At this point, however, we must consider several important nutritional concepts. Since DHA accumulates very fast in the human developing brain from the 32 weeks of gestation to the first postnatal months 12-19, any DHA deficiency should be corrected as soon as possible. This is a crucial concept that should be taken into account when devising a diet, since the processes that take place in the human brain during early development are very important and can be influenced by nutrition. These processes are the formation of synapses (synaptogenesis) and that of myelin (myelination). The former starts at 32 weeks of gestation, coinciding with sudden increases in most lipids and DHA 20-22. Myelin starts to be formed at about 35-36 weeks of gestation 23-24 and proceeds until much later, but it is the initial step that is important. During this time nutritional restriction or imbalance can cause a myelin deficit and some PUFA abnormalities 25-26. The retina develops even earlier, and DHA starts to increase at about 24 weeks of gestation 27, so that a nutritional restriction can reduce the retinal levels of DHA dangerously 12.
Since DHA deficiency is the main fatty acid abnormality in the brain in peroxisomal disorders, treatment should consist in giving a DHA preparation as pure as possible. This is the ethyl ester of DHA, better than 90% pure. The results obtained in as many as 30 peroxisomal-disorder patients treated with this preparation (in daily oral doses of 100-400 mg) project a ray of hope on the future of these children. The results of the treatment in the first 25 patients have appeared in successive articles 28-36 and the rest are going to be submitted for publication shortly. In contrast to the currently established dietary treatment, no fat restriction has been used with DHA therapy. For reasons specified earlier, a complete diet, as nutritious as possible for the age, has been given to all patients, with the only exception of green leaf vegetables and the fat in meat. This has not produced any undesirable increases in the two VLCFA 26:0 or 26:1. On the contrary, these VLCFA have decreased with the treatment, a proof that DHA deficiency is involved in the pathogenesis (mechanism by which a disease is produced) of peroxisomal disorders. Other important biochemical improvement has been the increase in red blood cell plasmalogen levels in most patients, again suggesting a cause-effect relationship between DHA deficiency and peroxisomal disease.
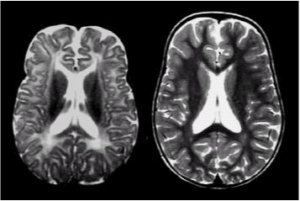
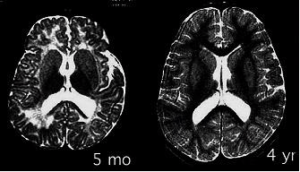
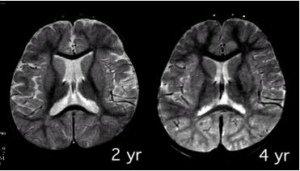
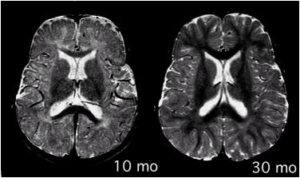
A most important improvement with DHA therapy has been that in brain myelin. This improvement has been repeatedly proven by MRI (magnetic resonance imaging) of the brain 31-33, 35, 36. Of the 17 patients in whom MRI follow-up was possible, a clear myelin improvement was detected in as many as 14 patients, and in half of them myelination totally normalized for the age. Figures 2 through 9 show some of the patients treated by M. Martinez, before taking the DHA-EE and after some time with the treatment, including their MRI scans.
Figure's 2,4,7,8
Figure's 3,5,7,9
Conclusion
Left untreated, generalized peroxisomal disorders are extremely severe diseases with a short-term lethal prognosis. Most patients die within the first years of life. However, treatment with DHA ethyl ester produces clear benefits to IRD/NALD patients. This therapy does not only correct their DHA deficiency but also increases their red blood cell plasmalogen levels and reduces their plasma VLCFA levels, without needing to decrease the nutritious quality of their diets. A growing child, whether healthy or not, needs to be properly nourished so that his/her brain can fully develop and myelinate. We believe that subjecting a child with a peroxisomal disorder to a fat-restrictive diet can only aggravate the situation. The brain is a fatty organ and needs an adequate supply of polyunsaturated fatty acids (PUFA) to develop. We have seen that peroxisomal patients have a most severe DHA deficiency. DHA is most important in the developing brain and retina. So we must always correct such a DHA deficiency without reducing the fat intake of the child. Doing the opposite (no DHA and a poor fat diet) will certainly shorten the life of peroxisomal patients.
The analytical and clinical improvements found in the DHA-treated patients suggest that DHA deficiency is an important factor in peroxisomal disease. At the very least, it can greatly aggravate the clinical course. Correcting peroxisomal DHA deficiency, on the other hand, clearly ameliorates the quality of life of these patients by improving their liver function, psychomotor development, vision and myelination. Thus DHA therapy should be initiated as soon as possible, before the damage is totally irrecoverable. We hope that in a near future, research on the causes for DHA deficiency in peroxisomal disorders and finding new ways to correct it may lead to further improvement of these patients.